MAIPA
Standardized Platelet-Antibody Screening and Identification
What is MAIPA?
Monoclonal Antibody-specific Immobilization of Platelet Antigen (MAIPA) is a qualitative technique for platelet antibody detection and/or identification. It is considered to be the gold standard method in the platelet immunology field.

MAIPA kits - 96T and 480T
Advanced Practical Diagnostics BV (apDia) has acquired the CE mark for the MAIPA Assay kit according to the Regulation (EU) N° 2017/746 regarding in vitro diagnostic medical devices (IVD) since 2023.
As the sole CE-marked MAIPA Assay kit available on the market, it stands out as a valuable alternative for laboratories currently reliant on Laboratory Developed Test (LDT) assays. This becomes particularly crucial in light of the impending restriction outlined in the European Regulation IVDR 2017/746.
The MAIPA Assay is available in two test formats 96T (REF 900006) and 480T (REF 900016).
The apDia ready-to-use human Platelet-Antibody Screening Cells & Platelet-Antibody Identification Panel Cells are manufactured by employing a special proprietary production process. The standardized antibody-screening panel allows the sensitive detection of anti-HPA antibodies, while the platelet antibody identification panel offers the ability to reliably identify the antibodies.
These reagents are advantageous for standardization, handling and workflow organization in the platelet immunology laboratory.
The use of well-characterized thrombocytes offers the ability to standardize the MAIPA: the apDia thrombocyte reagents allow the use of typed cells expressing even rare antigen combinations such as HPA-1 (a-,b+) [2.5%] and HPA-5 (a-,b+) [less than 1%] for an extended period of time.
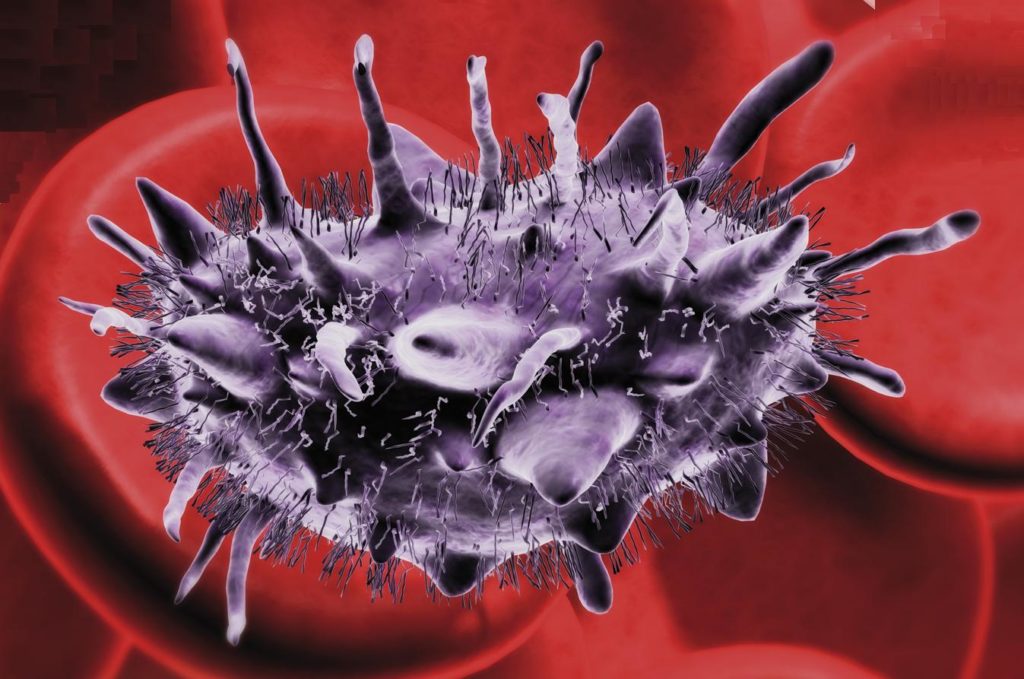
Detection and identification of allo- or auto-antibodies against platelets is indispensable for a targeted therapy of four clinical disorders in platelet immunology: FNAIT, PTP, PR and ITP in platelet transfusions.
- FNAIT
- PTP
- PR
- ITP
Fetal and neonatal alloimmune thrombocytopenia (FNAIT)
FNAIT can occur during pregnancy, when a mother gets immunized against platelet alloantigens present on fetal platelets. This may occur when fetal platelet antigens inherited from the father differ from and are not present on the mother’s platelets. Because of this immunization, IgG alloantibodies against the paternal platelet antigen are produced by the mother and then transferred through a neonatal Fc-receptor (FcRn)-mediated mechanism, crossing the placenta to enter the fetal circulation. The maternal alloantibodies can bind to the fetal platelets and cause immune destruction of platelets in utero. The ensuing fetal thrombocytopenia may lead to bruising, (intracranial) hemorrhage with possible associated neurological damage or even death in severe cases.
In Caucasian populations, FNAIT is most commonly related to anti-HPA-1a antibodies (approx. 85 – 90 % of cases) and to a lesser extent to anti-HPA-5b antibodies.
Post-transfusion purpura (PTP)
PTP is a rare transfusion reaction that may develop within two weeks after a transfusion of any blood product containing platelets (e.g. RBC concentrates) and can present as a severe thrombocytopenia complicated with bleeding and hemorrhage which can sometimes be life-threatening. It is most commonly identified in middle-aged multiparous women. All patients have had a previous sensitization to HPA alloantigens that they lack during a previous pregnancy or blood transfusion. The clinical condition of PTP is then mediated during a next transfusion as an antibody response against such platelet alloantigens in a second challenge (re-sensitization) to incompatible transfused platelets bearing the implicated HPA antigen(s).
As a result, the transfused platelets are destroyed by the produced alloantibodies, causing a sudden fall in platelet count. The most commonly implicated antibody is HPA-1a, made by HPA-1bb patients/recipients. Paradoxically, the patient’s own platelets are simultaneously destroyed through a not yet fully understood mechanism.
PTP is considered a self-limited disease with recovery of platelet counts in approximately 20 days. Treatment with IVIG (Intravenous Immonoglobulin) is regarded as the most optimal first-line therapy.
Platelet refractoriness (PR)
PR is defined as a condition of inadequate increment in platelet count following transfusion of random ABO identical donor platelets. It is a common complication in patients receiving multiple platelet transfusions. This clinical condition may develop when patients become immunized against HLA Class I antigens and make anti-HLA alloantibodies, leading to febrile, nonhemolytic transfusion reactions. Some patients may also develop anti-HPA antibodies with anti-HPA-5b the most common specificity. Because immunized patients often possess antibodies against different HLA Class I antigens, it can be diffucult to find compatible platelets
for transfusion support.
Immune thrombocytopenia (ITP)
ITP is also known as Idiopathic Thrombocytopenic Purpura. It is an autoimmune disease characterized by immune-mediated platelet destruction and inhibition of the platelet production. Affected patients make autoantibodies which destroy the patient’s own (autologous) platelets. In most cases autoantibodies against the platelet glycoprotein complexes GPIIbIIIa and GPIbIX are involved. Children may develop ITP after a viral infection and usually will recover without treatment. In adults, the disorder may be triggered by infection with HIV, hepatitis or Helicobacter pylori and may be a long term disease.
MAIPA PROCEDURE
BATCH DEPENDENT INFORMATION
Lot numbers can contain ‘-1’, ‘-2’, etc. these indications are for internal traceability. Content of certificates remain unchanged, based on the original lot numbers.
WANT TO GET IN TOUCH WITH US? NO PROBLEM!
- Call or mail us now.
- You get in touch directly with your contact person.
- You get a concrete answer for the next step.


